Radiation-induced Pneumonitis after Intra-arterial Radiation Therapy for Inoperable Hepatocellular Carcinoma
Case History

A 68-year-old woman presented with inoperable hepatocellular carcinoma in November 2000. She was treated with 6 cycles of adriamycin between November 2000 and March 2001, and achieved a partial response. Thereafter she underwent selective intra-arterial radiotherapy (SIR) with 90Yittrium microspheres in May 2001 with some response. She remained well for the following 4 months and then presented in August 2001 with a few weeks' history of shortness of breath and dry cough. On the day of admission, she experienced exacerbation of symptoms and sudden onset of palpitations. Her pulse rate was more then 200 beats/minute with a low blood pressure of 90/45 mm Hg. Oxygen saturation was 91% with 100% oxygen. Arterial blood gas later showed PO2 to be 11.6 kPa. Physical examination was otherwise unremarkable. Electrocardiograph revealed supraventricular tachycardia.
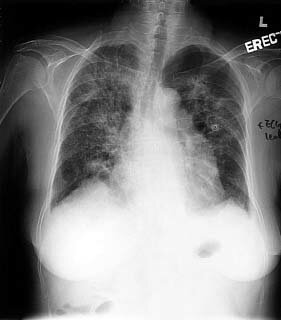
Chest X-ray showed diffuse bilateral lung interstitial changes with relative sparing of the periphery (Figure 1). The patient's heart rate was controlled at 100 beats/minute after injection of betaloc 5 mg and there was immediate symptomatic improvement. She was subsequently administered digoxin.
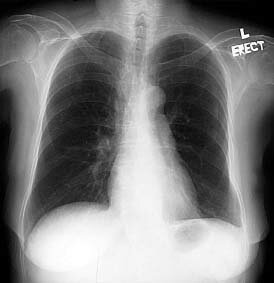
The patient remained dependent on high-dose oxygen during the next day despite the fact that there were no features of heart failure or chest infection. Echocardiogram was performed and showed good left ventricular function with ejection fraction of 60%. Given the patient's history of previous SIR with lung shunting of 10.8% 3 months previously, with a normal chest X-ray (Figure 2) prior to the procedure, the diagnosis of radiation-induced pneumonitis was made. An incidental finding of bilateral diffuse lung base infiltrate in a post-SIR follow-up abdominal computed tomography scan performed 1 week prior to the current admission further supports the diagnosis. A course of prednisolone 40 mg was started.
|
Figure 1. Chest X-ray showing diffuse bilateral lung interstitial changes with relative sparing of the periphery.
|
Figure 2. Normal chest X-ray following selective intra-arterial radiotherapy with lung shunting of 10.8% 3 months previously.
|
Discussion

Radiation pneumonitis is a known complication after treatment with SIR with 90Yttrium microspheres for inoperable liver tumours. It typically presents with symptoms of dry cough and progressive exertional dyspnoea without fever 1 to 6 months after SIR therapy (median, 3 months). The chest X-ray characteristically shows extensive patchy consolidation with well-defined lateral margins, sparing the pleura. Pulmonary function tests reveal a restrictive pattern. Lung biopsy, if performed, will show histological features of pneumonitis, with scattered microspheres readily detectable.
In a reported series, 5 cases of radiation pneumonitis were found among 80 patients who were treated with SIR therapy using 90Yttrium microspheres. Five of 9 patients (55.6%) with lung shunting >13% developed radiation pneumonitis, whereas this developed in none of those in whom lung shunting was <13% (71 of 80 patients). All 5 patients were treated with prednisolone 20 mg per day continuously. Symptoms improved in 2 patients, while the other 3 died of progressive respiratory failure.
Infective causes should be confidently excluded before steroid treatment is contemplated. The differential diagnosis will include infection, pulmonary oedema, pulmonary haemorrhage, and eosinophilic pneumonia.
References

1. Leung TW, Lau WY, Ho SK, et al. Radiation pneumonitis after selective internal radiation treatment with intra-arterial 90yttrium-microspheres for inoperable hepatic tumors. Int J Radiat Oncol Biol Phys 1995;33:919-924.
2. Lin M. Radiation pneumonitis caused by yttrium-90 microspheres: radiologic findings. Am J Roentgenol 1994;162:1300-1302.
Dr P Hui
Department of Clinical Oncology
Prince of Wales Hospital
Hong Kong, China
Dr MLS Chiu
Department of Clinical Oncology
Prince of Wales Hospital
Hong Kong, China
|
